Hand pathologies
ARTHROSIS
OF THE FINGERS

Summary
Diagnosis

Treatments
It's the degree of involvement, the extent of pain and joint degration, that will determine the best course of treatment.
Different treatments can be proposed for each stage of the disease.
Surgical treatment
In advanced forms of osteoarthritis, where the cartilage has disappeared, surgery is essential.
Several options are available, depending on the joints involved and their degree of damage.
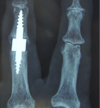
Prostheses
For metacarpophalangeal joints (at the base of the finger) and proximal interphalangeal joints (in the middle of the finger), prosthetic arthroplasties are preferred. These small prostheses provide good pain relief and can improve function in certain cases, depending on the severity of the preoperative damage and the healing quality of each patient.
Arthrodesis
For distal interphalangeal joints (at the tip of the finger, near the nail), arthrodesis is preferred, as it stabilizes the joint permanently, relieves pain and improves the aesthetics of the hand. Function may be temporarily impaired, but this segmental stiffness more than compensates for the functional impairment caused by the pain of osteoarthritis.
Isolated bone resections
In some cases, we can simply remove bone growths (osteophytes) or cysts that are satellites of osteoarthritis and peripheral to the joint. This is called an osteophyte osteotomy.
Generally speaking, this surgery is performed on an outpatient basis, sometimes using plexus block anesthesia of the whole arm, or in some cases, WALANT-type local anesthesia of the finger.
As a general rule, only your surgeon can discuss the various options with you, so that you can choose the one that seems best suited to you, since osteoarthritis can only be treated on a case-by-case basis, with tailor-made care.
Standard post-operative care
After these operations, nursing care is required every two to three days. Sutures usually resolve spontaneously within 15 days, but if they persist after this time, the nurse will be asked to remove them.
Occasionally, a postoperative splint may be used, but this is rarely the case.
Whatever the method, we recommend immediate mobilization of the finger which, in the case of prostheses, will be fixed in the bandage with the finger next to it - this is known as syndactyly. This provides a natural, mobile splint that promotes functional recovery.
The hand can therefore be used immediately within the limits of pain and without constraint for the first 3-4 weeks.
In the vast majority of cases, patients are able to use their hands for everyday activities within 3 to 4 weeks. Resumption of power and sports activities takes 4 to 6 weeks.
However, as every patient and every procedure is different, your surgeon will tell you precisely what you can and must not do.
Possible complications
Infections are exceptional in hand surgery, and when a prosthesis is fitted, antibiotic prophylaxis is systematically applied.
Algodystrophies are possible but rare in this type of surgery.
Stiffness may persist, with incomplete functional recovery, especially when the finger was very stiff before the operation, hence the importance of not intervening too late.
Fracture of the prosthesis is possible if the hand is used intensively. The implant can then be replaced.
Exceptional metal allergies can occur, as in the case of hip or knee prostheses. They manifest themselves as inflammation and pain that last an abnormal number of months after the operation.
In brief
Type of anesthesia
Sometimes plexus block, most often WALANT
Type of hospitalization
Ambulatory
Average downtime
No immobilization for prostheses
Average recovery time
Between 4 and 6 weeks for daily use, up to 3 months for sports and power activities.
RHIZARTHROSIS (osteoarthritis of the thumb)
Summary
Diagnosis

TREATMENTS
Medical treatment
Anti-inflammatories, analgesics and cortisone infiltration cannot cure osteoarthritis. At most, these treatments can relieve a painful flare-up.
Resting orthoses are often used in the early stages of the disease.
Hyaluronic acid injections can be used, but in early forms of the disease, Dr Couturier uses platelet-rich plasma (PRP). Injections are performed under local anaesthetic for the patient's comfort and under ultrasound control.
PRP can only act if there is cartilage remaining in the joint, because it is designed to improve the quality of this residual cartilage.
This method is performed in the clinic. Preparation and injection take about 30 minutes.
Surgical treatment
When medical treatment fails, or when the cartilage is so destroyed that the trapezium and metacarpal come into contact with each other, surgery is the solution of choice.
ARTHROSCOPY
This method can be used for less advanced forms that are resistant to medical treatment. Under anaesthesia of the arm, a small camera and small instruments are introduced into the joint to clean it and remove excess inflammatory synovium (synovectomy). Sometimes, small cartilaginous foreign bodies that have been released into the joint will also be removed.
This arthroscopy is sometimes combined with a PRP injection.
TRAPEZECTOMY
This was a commonly used method. The trapezium bone is removed. It is supplemented by the use of tendons to stabilize the metacarpal, which is then left without any support.
The after-effects of this surgery are long, with immobilization lasting 3 weeks, and patients often remaining in pain for several months. The thumb is shortened, and pinching with the other fingers may be impaired.
Dr Couturier performs trapezectomy only in extreme cases where prosthetic arthroplasty is not feasible.
TRAPEZO-METACARPAL PROSTHESIS
This is the most reliable and fastest method in terms of functional recovery.
The aim is to replace the joint between the trapezium and the metacarpal with a prosthesis that resembles a hip prosthesis. The principles are the same.
Surgery is performed on an outpatient basis, with anesthesia most often via plexus block (anesthesia of the entire arm) and sometimes under WALANT anesthesia to enable active mobility to be controlled during the operation.
Today, it is the gold standard in rhizarthrosis surgery.
Standard post-operative care
After arthroscopy, there is no thread on the scars, just steri-strips. These should be replaced every two or three days.
The patient can use his hand immediately, but without forceful activity for three weeks.
Sometimes, a thumb splint can be useful for 3 weeks if the ligaments have been re-tensioned during the operation.
Rehabilitation with physiotherapy is sometimes necessary.
After a trapeziometacarpal prosthesis, absorbable sutures are inserted and fall out on their own after 15 days. A nurse must re-dress the area every 2 or 3 days, and will remove the threads if they persist after two weeks.
On the day of the operation, a large bandage was applied to spread the thumb slightly. A few days later, this will be replaced by a removable, custom-made orthosis that takes the thumb.
This brace must be worn systematically at night until the postoperative check-up. During the day, it can be used for light-duty activities or when moving around in public places. The rest of the time, it is removed to enable the hand to be used for light everyday activities.
Most patients do not require rehabilitation, regaining full mobility on their own within two or three weeks. We have recently set up an early post-operative assessment protocol with a physiotherapist, enabling us to take prompt action on patients who have difficulty mobilizing on their own.
A post-operative check-up is scheduled three to four weeks after the operation.
Most patients return to normal use between the fourth and sixth postoperative week.
A hematoma is common at the base of the thumb or in the hand, sometimes in the forearm.
Swelling at the base of the thumb persists for 3 to 6 weeks, until internal healing has taken place.
There may be some disturbance of sensitivity in the back of the thumb, due to the spread of the small nerve branches at the time of the operation. This usually recovers spontaneously after a few weeks.
Possible complications
After arthroscopy,
tendon lesions have been described, but are rare in the literature.
Temporary stiffness may occur, sometimes requiring physiotherapy.
If pain persists, a prosthesis may be fitted.
After trapeziometacarpal prosthesis,
dislocation of the prosthesis is exceptional in the early postoperative period.
Early loosening of a prosthesis may be due to an allergy to one of its components, but this is exceptional, as in the case of hip prostheses.
The lifespan of such a prosthesis is currently 15 to 20 years, as we have only 20 years' experience with these implants. We can hope for a lifespan in excess of 30 years, as with hip prostheses.
Infection remains a rare complication of hand surgery.

IN SUMMARY
Type of anesthesia
Locoregional by plexus block
Type of hospitalization
Ambulatory
Average downtime
Partial immobilization (at night and during exertion) in a removable splint for 3 weeks.
Average recovery time
Back to light everyday activities in 1 week to 10 days.
Return to strength and stress activities (strength training, sports) around the sixth postoperative week.
Carpal tunnel syndrome
Summary
Diagnosis

Treatments
It's the degree of damage, the extent of nerve compression, that determines the best course of treatment.
Different treatments are proposed for each stage of the disease.
Surgical treatment
When medical treatments no longer work, or when the nerve shows too much damage on the electromyogram, or when paralysis sets in, surgical treatment is necessary.
The aim is to enlarge the carpal tunnel by cutting the ligament that covers it: the annular ligament.
Dr. Couturier uses two methods to achieve the same results. The procedure is performed as an outpatient or in an Office Surgery.
Endoscopic carpal tunnel surgery
A small camera is inserted into the carpal tunnel, allowing the annular ligament to be severed under visual control.
This surgery can be performed under locoregional anaesthesia using a lexical block, or using an innovative anaesthesia technique known as the WALANT method.
It allows much faster recovery of function.
Ultrasurgical carpal tunnel surgery
A small knife is slid along the annular ligament to cut it. Control is performed under ultrasound.
This surgery is mainly performed under WALANT anesthesia.
The French health authority has issued a recommendation for the management of this disease. Discussions with your surgeon should be held on a case-by-case basis, to tailor the treatment to your needs.
Standard post-operative care
Skin sutures are usually omitted. Steri-strips are replaced by a nurse and removed after a dozen days.
In the immediate aftermath of carpal tunnel syndrome surgery, tingling and nocturnal pain should disappear on the first postoperative night.
There may still be a sensitivity deficit, or even a motor deficit, for several weeks if there was such a deficit before the operation. This is linked to nerve regrowth, which can take several months in some cases.
Occasionally, you may experience electric shocks when using your hand. Don't worry, this usually disappears within a few weeks.
Usually, the heel of the hand is a little tender due to the internal scar made on the ligament that was severed to free the nerve. This may last several weeks, but is normal.
Possible complications
There may be a lack of sensitivity or mobility of the definitive thumb if the operation was performed late and this paralysis existed before the operation. Recovery is not always complete.
Sequelae may be permanent if the operation is carried out too late.
Algodystrophy is always possible in the aftermath of any surgical procedure.

In brief
Type of anesthesia
WALANT In most cases
Type of hospitalization
Ambulatory or Office surgery
Average downtime
No post-operative immobilization, immediate and careful use of the hand
Average recovery time
From 10 days to three weeks on average, sometimes several months depending on your healing.
Dupuytren's disease
Summary
Diagnosis

Treatments
Several treatments are available. Not all of these treatments are available in France.
Depending on the extent of the disease, treatment options will be explained to you at the consultation, but it's up to you to choose the method you prefer, based on the explanations you'll be given and the chances of success.
Standard post-operative care
Cutaneous sutures are made with sutures that absorb spontaneously after a fortnight. Sometimes a nurse will have to remove them if they do not absorb.
Dressings should be applied regularly every two to three days to keep the wound clean. The skin may appear whitish, as if you've been in the water too long. This maceration is not uncommon after surgery, especially when local reconstruction techniques (flaps, skin grafts) have been used.
Dr. Couturier does not recommend immobilization; on the contrary, patients should use their hands immediately to try to maintain the finger extension achieved during the operation.
Physiotherapy or dynamic orthoses may be added immediately postoperatively, or after the first postoperative check-up.
It is common to have a hematoma in the palm of the hand or under the small flaps made for microsurgical reconstruction.
Possible complications
Recurrence, which is not a real complication, is frequent in this disease, especially when there is an alcohol/tobacco association.
Often, the disease spreads to another finger, or further on to the operated finger.
When a patient has undergone multiple operations on the same finger, there is a risk of ischemia of the finger (consequent reduction in vascularization), which can lead to amputation of a fragment of the finger.
Occasionally, large hematomas in the palm of the hand can slow healing and hamper postoperative mobilization.
Infections are exceptional in this disease.

In brief
Type of anesthesia
Plexus block or sometimes WALANT
Type of hospitalization
Ambulatory or Office Surgery
Average downtime
No immobilization required. Immediate mobilization of fingers.
Average recovery time
Between 3 and 6 weeks on average for function, up to three months for scar softening